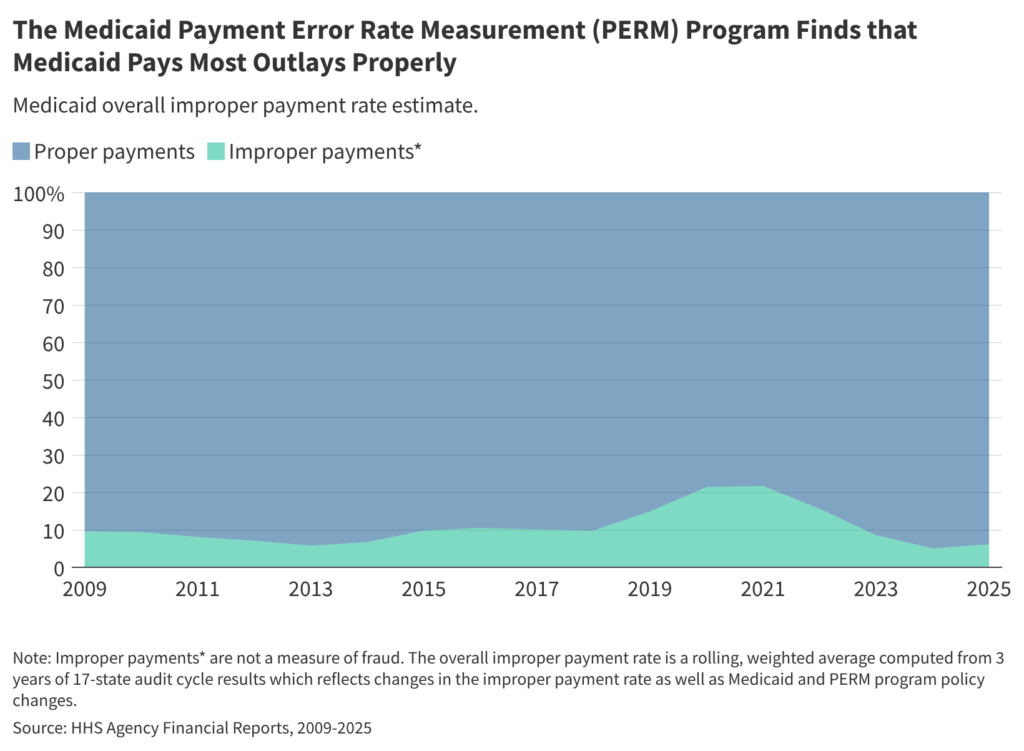
Box 1: The improper payment rate has changed over time, largely due to the ACA implementation and the COVID-19 public health emergency.
Pre-ACA: Between 2009 and 2013, the overall improper payment rate trended downward as information systems improved states’ ability to determine provider and enrollee eligibility . The PERM program’s eligibility component error rate decreased from 2011 to 2014, when it was estimated at 3.11 percent (Figure 3). The Patient Protection and Affordable Care Act (ACA) passed in 2010 and phased in several changes to the Medicaid program, including the 2014 Medicaid expansion.
ACA Implementation: During the 2013-2019 period, the overall improper payment rate trended upward, driven by errors in FFS claims related to state non-compliance with new provider screening, enrollment, and documentation requirements introduced in 2012 under the ACA. From 2015 to 2018, HHS suspended eligibility audits as states began to implement new eligibility standards and determination requirements under the ACA. During this period, the overall PERM rate was calculated using a proxy eligibility estimate of the 2014 eligibility component error rate, 3.11 percent to provide states with time to adjust to eligibility process changes in the Affordable Care Act.
Post ACA: Beginning in 2019, PERM reintroduced the eligibility component under updated rules, for the first time requiring states to work with an independent contractor using nationally standardized eligibility audit procedures2. Between 2019 and 2021 the overall improper payment rate rose again (Figure 3), driven by the new standardized PERM eligibility audits. Most of the eligibility error rate was attributed to errors due to insufficient documentation or administrative mistakes. The 2021 improper payment rate is the first estimate that includes reintegrated eligibility error rates (conducted under updated rules) for all three audit cycles (i.e., all states).
COVID-19 Public Health Emergency (PHE): Beginning in 2021, the overall improper payment rate decreased sharply. In 2024, the improper payment rate (5.1%) was less than one-fifth of the 2021 estimate (21.7%). The 2024 improper payment rate was the lowest rate since the COVID-19 pandemic began, which HHS reported was due in part to the exclusion of certain audit review elements as policies adopted during the PHE that paused eligibility renewals and disenrollments and reduced requirements for provider enrollment and revalidations were taken into consideration and due to improved state compliance with program rules. The COVID-19 PHE and related flexibilities were in place from early 2020 through early 2023.
Post-COVID-19 PHE: In early 2023 states began to phase-out the continuous enrollment provision that suspended Medicaid eligibility renewals and disenrollments during the pandemic and flexibilities that reduced provider enrollment requirements. Most states completed eligibility redeterminations for all Medicaid enrollees and resumed disenrollments by August 2024. Improper payment rates since 2021 include at least some audits conducted while COVID-19 PHE flexibilities were in place. The 2025 improper payment rate incorporated the first full audit conducted following the end of the PHE (July 2023 – June 2024). The 2025 improper payment rate (6.1%) increased relative to 2024 (5.1%). From early 2023 through late 2024, states resumed eligibility renewals and disenrollments and phased out provider screening flexibilities allowed during the PHE.